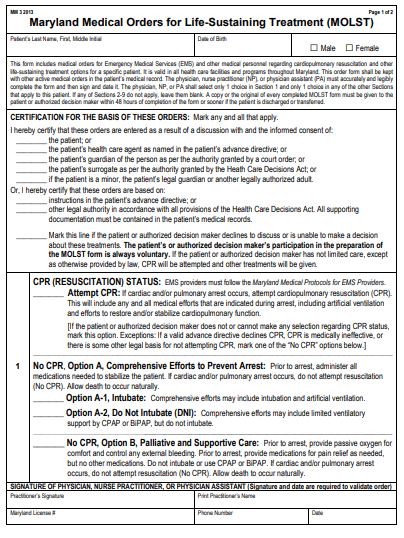
On the first page of the Maryland Medical Orders for Life-Sustaining Treatment, or MOLST, there is a section for people to choose if and how they would or would not want CPR.
There are many people who have an advanced or life-limiting illness who would not want to be resuscitated should their heart stop beating. There are also many people who aren’t aware that this wish cannot be honored without an important document – the Medical Order for Life-Sustaining Treatment, also known as a MOLST. In Maryland, emergency responders and other medical personnel are required to perform CPR on a patient whose heart has stopped unless they are aware that person has a MOLST stating that it is not to be performed. This form is only valid if signed by a physician, nurse practitioner or physician’s assistant.
It isn’t as simple as checking off one box – the form addresses many other life-sustaining measures that people may or may not want to exclude from any care when facing a medical crisis, including administering antibiotics, performing dialysis and using artificial ventilation. That is why it is important that patients and their families review the form with their provider as it is written in medical vocabulary that needs to be discussed in terms that can be understood. It might be a good idea to review the form and write down questions before talking with your provider. You can download the form at www.whymolst.com/resources. In this article, we are going to review Section 1, which addresses resuscitation.
The first option in Section 1 is “Attempt CPR”. That means that all comprehensive efforts will be made in the event of a cardiac arrest. If one’s heart stops, responders will perform chest compressions, they may place a breathing tube, administer medications and defibrillate or use electricity to try to restart the heart.
Full code patients will usually be transferred to an emergency department or higher level of care such as an intensive care unit. There are some risks involved with CPR, including fractured ribs or damage to internal organs. Even if someone is successfully resuscitated, there is always the risk that one will experience a level of debility because vital organs such as the brain have gone without blood flow.
Section 1’s next options are for no CPR. “No CPR, Option A, Comprehensive Efforts to Prevent Arrest” means all comprehensive efforts will be made, including administering medications, but there will be no chest compressions if cardiac arrest occurs. Option A is further broken down into two choices: “Option A-1, Intubate” or “Option A-2, Do Not Intubate (DNI).”
Selecting Option A1 means a breathing tube can be used and the patient can be placed on a breathing machine. Selecting Option A2 means they will not use a breathing tube but can use a CPAP or BiPAP machine. CPAP and BiPAP are devices that provide positive airway pressure therapy using a mask that covers the nose or nose and mouth which delivers compressed air to open and support the airway. Again, selecting Option A1 or A2 informs the medical team that should a patient’s heart stop, there will be no CPR, allowing death to occur naturally.
Electing the “do not resuscitate” option does not mean that the medical team will stop all treatment. The care team will continue to treat the patient and their condition until their heart stops beating. Instead of thinking of DNR as Do Not Resuscitate, consider it to mean Die Naturally with Respect.
The final option regarding resuscitation is “No CPR, Option B, Palliative and Supportive Care.” That means if a person were to have a cardiac arrest, the medical team would make sure the patient is comfortable and free from any disturbing symptoms like pain, shortness of breath, and anxiety. They would provide oxygen through a nasal cannula, but they would not intubate or use CPAP or BiPAP. When the heart stops, they would allow the patient to die naturally.
Electing the “do not resuscitate” option does not mean that the medical team will stop all treatment. The care team will continue to treat the patient and their condition until their heart stops beating. Instead of thinking of DNR as Do Not Resuscitate, consider it to mean Die Naturally with Respect.
Watch this community education video to learn more from Dr. Sherman about Section 1 of the Maryland MOLST form:


